An Interview with Mit Desai, MD, FACS – CEO & Founder of The Surgicalist Group
[Surgeon-preuner and Healthcare Change Agent]
By Lynn Purdy, Chief Marketing Officer
During the time of the COVID-19 pandemic many are finding ourselves working from home and prioritizing work that could be done remotely. In my case, I was able to do an in-depth interview of our CEO and Founder, Dr. Mit Desai last week using the #Microsoft365 Teams app and were easily about to comply with the 6 feet of social distancing guidance by utilizing VOIP and video sharing. It was the perfect way to get to know him better and explore our business model. The interview also helped Dr. Desai prepare for The Healthcare Solutions Project podcast that aired on March 16, where he was a guest (and first physician ever) on the program. You may listen to the podcast by clicking here).
Q: Why did you decide to get into healthcare? And what was it that shaped your current focus?
Growing up in an Indian family, there were only a few professions that are encouraged… engineering, law, and medicine are at the top of the list. I was always interested in science and pursued a degree in microbiology as an undergrad at University of Michigan and graduated with honors. I set my goal on going to medical school early on. Initially I thought I’d like to pursue ophthalmology, in fact between undergraduate training and medical school, I did research in ophthalmology. However, during medical school, I had a rotation in general surgery and fell in love with it. I still remember the exact moment when I realized I had to be a surgeon. I did an internship at Cedars-Sinai in LA and then my General Surgery residency at UIC-MGH in Chicago, not too far from my home in Michigan. I trained as a general surgeon and went into private practice initially in Naples, Florida. I wanted to get far away from the snow and cold of the Midwest – that was back in ‘03. It was an adventure my wife and I went on together, that started small but grew into something much larger than our original intent. I started what would eventually become The Surgicalist Group in 2007.
As for shaping my current focus, The Surgicalist Group business grew out of the reality that after practicing as a general surgeon for 4 years, my life was consumed with building my practice, taking call at a number of hospitals in the Tampa area, which meant I was working 24 hours a day, 7 days a week 365 days a year. Infact, I didn’t take a vacation from 2003 to 2008. For general surgeons, it’s not unusual to get calls in the middle of the night and have to spring into action anytime there is an emergency to take care of a patient who needs surgery. It takes a toll on general surgeons. I saw friends whom I trained with who went into private practice as general surgeons who had challenges managing their lives. I enjoyed the entrepreneurial aspect of what I was doing building my practice, but I also knew that life wasn’t sustainable if I wanted to keep my family and marriage intact, as well as my own physical and mental well-being. I realized I needed to find a different strategy. At the same time, I also recognized the way hospitals were managing emergent and urgent surgery wasn’t optimal. Many patients who should have surgery are either boarded for hours or days until a community surgeon is available. This introduces its own set of issues including clinical risks and patient dissatisfaction. The emergent surgery service is surgeon-centric, not patient-centric. The outcomes around quality, efficiency, safety, and cost of care were not getting the attention they deserved. And, hospitals were paying for a surgeon to be on-call but not really getting the type of service they were paying for or wanted, for that matter.
That lead me to an epiphany I had that started The Surgicalist Group business. One day, I was having lunch in the hospital with a hospitalist, which is an internal medicine doc who doesn’t have a private practice and works 12-hour shifts. They typically have a day shift and night shift to cover the hospital inpatients. I tried to imagine a way that could apply to general surgery. To elaborate on the hospitalist model, it’s based on managing the care for patients who are admitted to a hospital for an acute care episode – to treat pneumonia, for example. The hospitalist manages the care of the patient while they are in the hospital, including bringing in specialist for consults and keep the primary care physician informed of their patient’s status. The hospitalist is essentially the gatekeeper for that patient while they are in hospital. They coordinate discharge and send them home or to the next site of care and transition downstream care management responsibilities with their primary care doc. In addition to managing the acute care episode, hospitalists also partner with the hospital to drive performance improvement. They were essentially ambassadors in the hospital to change the way inpatient care was managed. While they were doing important clinical work, they were also making changes to help fix a broken healthcare system. As I listened to the hospitalist talk about their work and the fact that they worked block schedules of 12 hours on and 12 hours off, it gave me the idea that this could work for general surgeons, too, if we just focused on emergent and urgent care. Certainly not with a 12 hours on/off schedule but something else that would be amenable to general surgeons. I could create a surgicalist practice that would help the hospitals get more value for the money that they were spending for on-call surgeons and locum tenens staffing and become a change agent within the hospital on the general surgery side of the ledger, while also creating a better quality of life and a new purpose for general surgeons.
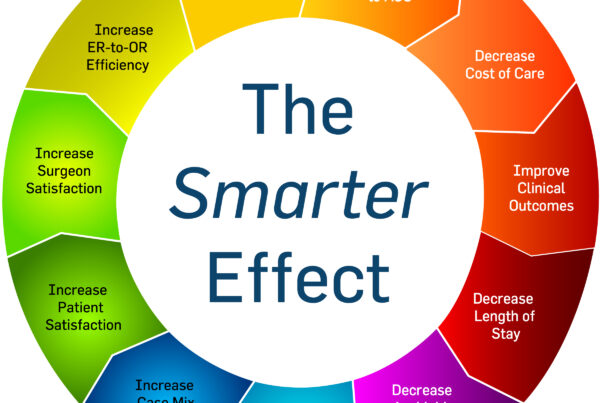
We’ve evolved since the practice started with emergent and urgent surgery. Today we also provide trauma surgery with surgical critical care, as well as wound care and procedures like starting lines and other invasive procedures. In our evolved model, we now implement evidence-based protocols and workflows designed to drive improvements in quality, efficiency, patient satisfaction, and cost of care. We are partners with the hospital to improve the value of the care provided.
Q: What is a challenge that the health care system is facing today that should be on the mind of every healthcare leader today?
Every hospital is working to improve their performance and deliver on the value-based purchasing objectives introduced by CMS about a decade ago under the Affordable Care Act. There has been plenty of focus on the inpatient care medicine side of the scorecard for the acute episode of care from the ER to post-discharge from hospitalization episodes. Surgery has had some value-based objectives set by CMS, but these are limited in scope compared internal medicine. For surgery, CMS has mandated value-based guidance around hip / knee replacement outcomes and for colon surgery (colostomies, colectomies, bowel resections, etc), which impacts our practice. Since one of the biggest healthcare expenditures for CMS and other payors is around surgery, this is a big opportunity for improvement. The US healthcare spending increased 4.6% to $3.5 trillion or $11,172 per person and accounted for 17.7% GDP. Hospital expenditures grew 4.5% to $1,191.8 billion in 2018- which was slower than the 4.7% growth in 2018. Hospitals still have work to do in the surgical services arena and that’s where we can help them, as a surgeon-founded and led organization. We have the best interests of the patient, hospital, community general surgeons, and the surgical team.
Q: How is our organization approaching the challenges we just discussed?
Optimizing operations for surgical services is an area that most hospital administrators continue to try to get their arms around but haven’t been successful is addressing it with typical top-down mandates. With a surgeon led organization, coupled with evidence-based protocols and workflows to drive improvement in the system, we identify where the gaps are in the workflows and how to drive change. It’s around getting alignment in the ED and OR, focusing efforts on implementing lean strategies, standardization, allocating block time, and standardization on approach and supplies. While it seems low-tech, it is. The innovation comes in around execution and the people delivering care having accountability, transparency, and a service-minded approach. Using data to measure performance helps us become more efficient and effective and often has an up-tick effect within the hospital where we practice.
Technology does have a role but it’s just part of the overall solution that makes us more efficient. Every surgeon uses a mobile device to enter the work they’ve done for charge capture. They have knowledge of how to accurately document what they’ve done and then we have a team of coders who confirm they have the appropriate information entered that represents the work and the acuity. Making it easy for the surgeons is key. I’ve personally done every job in the organization and I taught our surgical leaders and back office teams how to be as accurate and efficient as possible.
Q: Describe what makes our surgicalist solution innovative.
Our teams are effective because we are aligned with the hospital’s goals and the transparency in performance keeps us all accountable. But we are also about looking at how to work smarter (not harder) through innovation. In fact, we have a webinar coming up with the Becker’s Hospital Review on April 14 about adopting concepts from research done by Drs. Vijay Govindarajan and Ravi Ramamurti for their recently published HBR book, Reverse Innovation in Health Care. Their research studied innovation implemented in developing countries like India that have enabled them to address the healthcare needs for large populations of people more efficiently with high quality outcomes and lower cost than we can in the US. A few examples include the concept of focused factories, where a hospital focuses on one surgical specialty and refines its processes to the Nth degree to bring standardization and optimization to surgery. For example, there’s a hospital in India that provides eye surgery and can complete cataract surgery at 0.3% of the cost as it is in the US with equivalent outcomes. This is because they have fine-tuned their processes and supply chain so well that they can drive cost down and get the most efficiency possible out of their processes.
General surgeons are trained to operate a wide variety of body systems spanning the digestive system (the esophagus, stomach, intestines, gallbladder, spleen, liver, pancreas, kidneys), breast, skin, and soft tissue, as well as the endocrine system (the thyroid, pituitary, and adrenal glands). We are also trained in surgical oncology and trauma. Some general surgeons go on to subspecialize in those areas. In our case, we are focused on a limited set of general surgical procedures that typically fall into the emergent and urgent category – common surgeries like removing necrotic gallbladder or appendix, or removing a perforated colon, or fixing a strangulated hernia that is causing a bowel obstruction. In our practice as surgicalists, we focus on emergent and urgent surgeries only. That means the highest volume of the most common emergency surgeries are handled by our team. In that way, we are a type of focused factory inside the hospital. Our surgicalists get very good at performing a narrowed scope of emergent surgeries which improves the hospital’s ER and OR efficiency, clinical outcomes, and costs of care with a narrow cohort of patients. We are also experts in reducing complications and can help reduce avoidable readmissions to the hospital which can be costly.
Another concept in the reverse innovation model is leveraging a hub and spoke model, which we do as well. Most of our work is in the community hospital arena. However, in some communities, where there is a critical access hospital within a reasonable distance to us, we can provide coverage for that hospital or refer the patient from the critical access hospital to the community hospital for surgery. We also provide support for some of the local long-term acute care hospitals that need us, where it’s much better for the patient if we can provide the care there versus moving them to an acute care hospital across town. Often patients in LTACs have complex care needs that make moving them costly and risky. Patient and family satisfaction of having a surgicalist on-site is important in the long-term acute care setting.
Q: Describe the benefits that our solution offers to hospitals, health systems, payers, and employers.
One of the biggest value drivers we bring to the hospital is addressing the acute care needs for patients, ensuring they receive the right care, at the right time, and the right place. We aren’t about putting off to tomorrow what can be done today. And, as we’ve discussed, we are also helping the hospital improve throughput in the ED and the OR. The adage of time is money is very true in hospitals and especially in the surgical services area. Getting the patient in and treated as quickly as possible is important for hospital operations but it’s also important clinically. But looking at the business side for a moment, an hour of OR time is costly at $62/minute (OR costs ranged from $22 to $133 per minute, depending on the complexity of the procedure, with an average cost pegged at $62 a minute, according to an older study of 100 hospitals in the United States (J Cosmetic Surg 2005;22[1]:25-34). Here’s another article that talks about cost vs charges JAMA Op-Ed). Basically, the more efficient the hospital can be the better it is for everyone involved, starting with the patient. But it’s also better for the hospital and the surgeon.
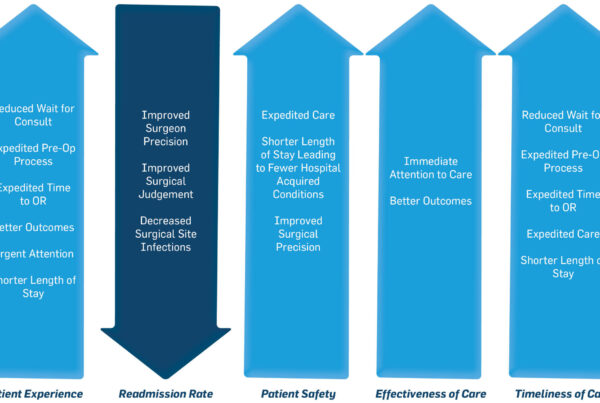
From a payor perspective, we understand their goals of getting the patients treated as expeditiously as possible, reducing complications, and getting them discharged to the next site of care as quickly as possible. With most of our emergent and urgent surgeries for removing a gallbladder or appendix, the patient can go home safely the same day. We have a physician assistant on staff who is high touch with the patients before and after surgery. Part of their role is to ensure the patients are discharge home safely or the most appropriate next site of care. They also ensure patients have the right follow up care with their primary care physician. They key is communication and coordination which we have fine-tuned in our model. Our teams are committed to add value through the healthcare supply chain, for the patient, for the hospital, for the payor, and for the staff – including the surgeons.
Q: Tell me how our solutions benefit patients?
There is the challenge every hospital is addressing and that is improving the patient experience of care. From an emergency surgery standpoint, the patient’s experience of care typically starts in the emergency department. When a patient comes in with abdominal pain and is determined to need a gallbladder or appendix removed, and there is a dedicated surgicalist available 24/7 365 days a year, the patient experience goes way up. Everyone has heard stories or had experiences with cases like these where the patient is sent home with a handful of prescriptions to manage pain and antibiotics for infection and told to follow up with the community general surgeon at their next available appointment, which can be days. In the interim, they could have another acute attack and go to another ER and have their gallbladder out. There’s the risk of complications and the reality that the hospital’s indexed case capture goes down and they lose the ability to treat the patient on the first point of contact with the hospital in the traditional ‘surgeon-centric’ model. Our model is patient-centric and hospital-centric.
Q: Let’s talk about what results we’re seeing from our services? Can you offer any examples of how our organization has created results in the areas of improved outcomes, lowered costs and patient satisfaction?
We can help the hospital drive their surgery volume by creating a reputation for being ‘patient-centric’ and ensuring that when patients need surgery, they receive the right care, at the right time, and right place. We also free up the community surgeons to focus on their elective practice and offload the urgent/emergent cases to our teams. Hospitals are paying community surgeons to be on call and it’s not uncommon for the community surgeon to have the ED discharge the patient home on pain meds and antibiotics and have them come into their clinic another day that suits the surgeon’s schedule – a ‘surgeon–centric’ model. In the meantime, the patient is not the central focus and the hospital is managing risk. They are also paying the on-call physician up to a couple thousand a day whether they come in or not. We eliminate that situation and provide the service to the hospital for their community 24/7, 365 days a year.
In a study by Oliver Wyman, we were able to decrease average length of stay by 8% for appendectomies, and 24% for cholecystectomies. We also demonstrated a 47% reduction in 30-day readmission rates for our cases, and reduction of 22% in complication rates for our cases. In addition, the American College of Surgeons has validated the surgicalist model demonstrating that surgicalists help decrease the overall hospital costs by 31% with an estimated $2MM a year in savings for hospitals implementing a surgicalist model. They also saw a 43% reduction in the rate of complications (which also reduces cost/case), and a 27% readmissions rate and 9% reduction in the average length of stay.
Our team also analyzed our performance around operative cases performed per call day before and after implementing a surgicalist service from one of our community hospitals. We were able to more than double the number of operative call cases performed/day with a 128.8% improvement (0.80 to 1.83). Carving out the hospital’s index case capture for cholecystectomy, we were able to show an increase of 169.2% (0.26 to 0.70) – meaning the patient who came into the hospital and needed their gallbladder removed had it done that day verses sending the patient home and doing it on a subsequent day by a non-surgicalists. In addition, the income generated from increased cholecystectomy and decreased length of stay together showed a 24.65% improvement in revenue for the hospital ($4,531 to $5,648 – which annualized would be $>2.4MM of incremental revenue). We’ve also surveyed EMS teams that deliver patients to EDs and the results show us that 96% felt they’d prefer bringing emergency cases to those hospital where our surgicalist work because they know the surgicalist will be there and manage the patient efficiently and without begging or pleading for them to come to the hospital.
Q: What is your proudest experience you have experienced to date?
That’s a tough question…I don’t really think like that. Certainly, I’m excited about being able to help as many patients as possible and expanding this surgicalist model will help do just that. Being a general surgeon, it’s probably engrained in me to help people and recently I’ve been on a couple of surgical mission trips to India where I’ve been able to help many patients get care that they otherwise wouldn’t have received.
I’m am proud of the fact that we’ve been able to recruit incredible surgeons who love our surgicalist model and are so engaged. In fact, since 2007, we have a greater than 90% retention rate for our surgeons which is unheard of! Most importantly these surgeons have been able to live a full life with surgery just being one part of their life instead of it being all consuming.
Q: If you could wave a magic wand and change something about healthcare today, what would that be?
I’d like to make sure every hospital C-suite member knew about the value of surgicalists and what we can bring to their hospital. It’s a very new sub-specialty and many people don’t know about the value surgicalists can bring to their communities yet. For small organizations like ours without big budgets for advertising, getting the word out really would benefit from having a magic wand!
Q: What do you think it will take to heal the healthcare system in this country?
We absolutely need to look at what’s happening in developing countries and consider how to bring the ideas that are disruptive, like reverse innovation and ensure we are paying for value, not volume. I believe competition is good and the numbers don’t lie. When you have transparency and data, it’s hard to argue that changes like we’ve adopted aren’t relevant.
Q: How can hospital administrators who are interested in exploring our surgicalist model (or general surgeons who are interested in becoming surgicalists) get in touch with you?
Drop an email to me in care of this email address info@thesurgicalist.com or call 813-940-SURG.