Written by Casey Thomas, DO, FACS, FACOS, Chief Medical Officer for The Surgicalist Group
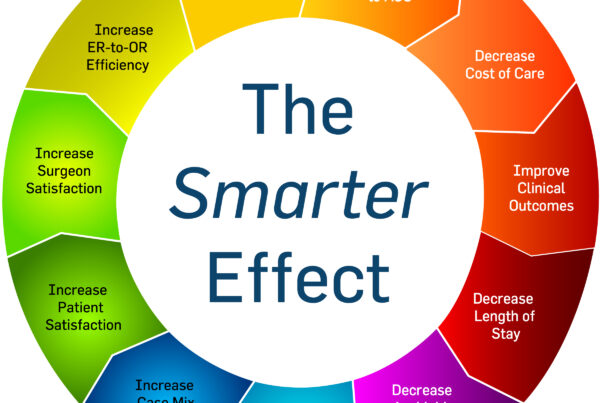
As healthcare workers, we constantly hear about optimization, improving the care we provide and containing costs. Usually we think of these as isolated processes, however, in the unique world of the acute surgical patient, poor optimization has a far-reaching impact that can mean the difference between a positive experience for the patient and a profitable encounter for the hospital to horrible patient satisfaction and hospital revenue loss.
We often establish treatment protocols and algorithms based on medical patient admissions. We streamline testing and labs; we have nursing driven treatment protocols to speed up diagnosis and treatment of common medical issues. The treatment, throughput, and billing for medical patients has become extremely efficient since the advent and implementation of hospitalist services. Separating outpatient and inpatient medicine revolutionized the treatment and outcomes for medical patients.
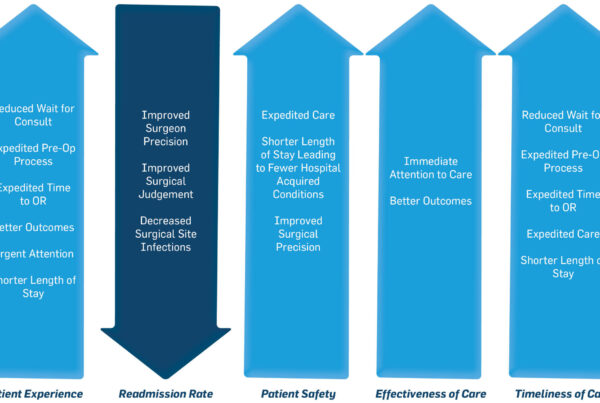
Acute surgical patients impact the efficiency of a hospital to a much greater degree than medical patients. For most acute surgical patients, the only issue requiring their stay in the hospital is their need for surgery. The majority of revenue the surgical patient generates comes from his/her operation. The longer their length of stay, the less revenue that patient generates.
There are multiple areas where a dedicated surgicalist can optimize a patient’s hospital stay due to their singular focus of caring for in-house patients. Evaluation in the emergency department (ED) does not have to wait until the end of clinic – this expedited consultation allows for earlier operating room (OR) availability. The surgicalist can utilize any unfilled slots in the OR schedule that might have otherwise gone unused – thus improving OR utilization. The ability to round early in the day and discharge patients as soon as they are ready – not having to wait until elective cases are finished, ultimately optimizes care and decreases the length of stay for the patient. Under the classic model of surgical care, the ED waits for the surgeon, the OR waits for the surgeon, the patient waits for the surgeon – all leading to decreased optimization of care.
The ramifications of all these delays frustrates patients, other healthcare providers, and leads to inefficiencies and loss of revenue. The hospitalists solved these issues and optimized the care of medical patients decades ago. By applying the same principles, we have seen be so affective with medical patients, we can improve the care, outcomes, and profitability with surgical patients.