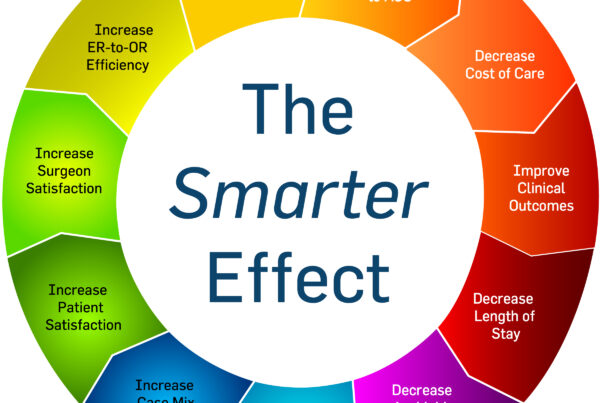
If you have heard about surgicalists and are wondering how they could be a beneficial service for your hospital, there’s no better time than now to understanding the impact they can have on your hospital program. As we emerge from the COVID-19 pandemic, hospitals eager to regain lost revenue, will welcome elective surgical cases back into their ORs. Focusing on their own practice, community general surgeons will be working through a backlog of elective surgeries, making emergency surgical call coverage even more difficult to manage. For many hospitals depending on community surgeons to cover surgical call, this may be a great time to introduce surgicalists into the equation. There are several benefits to implementing Surgicalists in your hospital.
Here are a few reasons how implementing surgicalists can be beneficial to your hospital program:
1. 24/7 Acute Care Surgery Coverage/Continuity of Care
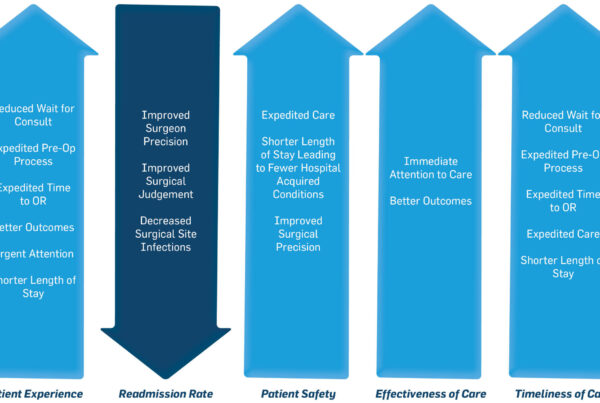
When surgicalists can offer 24/7 dedicated coverage for emergency surgeries vs. an on-call surgeon, it looks much different to the patient and to your bottom line. Our surgicalists provide dedicated coverage for emergent and urgent surgical cases. They don’t have an elective practice. And so they are there for your patients when they need them most. There is no waiting for the on-call surgeon. Our surgicalists are there, in your hospital, 24 hours a day, 7 days a week.
Having a surgicalist readily available lessens the time your patients wait for proper care. Instead of waiting hours, or sometimes days if discharged, they can receive the urgent surgery they need on that same day. Treating their condition immediately prevents further deterioration of their condition, allowing the surgicalist to discharge them the next day following surgery.
For the hospital, the less time a patient spends at the hospital, or the shorter the length of stay (LOS), the fewer resources are used to care for that patient. Supplies and overhead from custodial workers to nursing teams all add up quickly in each day spent at the hospital.
2. Enhanced ER-to-OR Efficiency
When surgicalists make themselves available to a hospital 24/7, they enhance efficiencies in every area the patient touches, but make their greatest impact in ER-to-OR efficiency. Working hand-in-hand with the emergency department and operating room, our surgicalists integrate their services into the daily workflow of the hospital. Each day they connect with the operating room scheduler to understand gaps in block schedules, timeframes where they can fit in an unscheduled emergency case. Additionally, they collaborate with the emergency department, ensuring processes are in place to expedite surgicalist consultations as they are needed.
In an on-call scenario, patients needing urgent or emergent surgery can wait hours to see the surgeon on call, who is most likely waiting to finish his elective practice appointments first. While the patient waits to be consulted, they are using a bed in the emergency room that could otherwise be utilized by others needing emergency care. By the time the surgeon is able to meet with the patient and then find time in both the OR’s schedule and their own, the surgery often does not occur until the next day, at earliest.
There is a better way – the surgicalist way. With surgicalists readily available to consult patients in the ED and take advantage of down-time in the OR, emergent and urgent surgeries happen the same day the patient arrives in the emergency room. With the surgicalist model, patient care occurs in a timely manner while utilizing hospital resources already available.
3. Relieve Community Surgeons of Call Coverage
Across the nation, community general surgeons are resuming their elective surgical cases that have been building over the past several months under the guise of the COVID-19 pandemic. Flooded with patients waiting for surgery, their days are long as they manage in-office consultations and begin to book elective cases in the OR. On top of this hectic schedule, many have to manage emergent and urgent cases that occur when they are on call.
Under the surgicalist model, surgicalists relieve community surgeons of their on-call burden, allowing them to focus on their private practice and elective cases. In doing so, community surgeons make the most of their time, take better care of their patients, and have a better quality of life – absent from the stress of managing both elective and on-call surgical cases.
For hospitals, this ensures all patients receive the right care, at the right time. This is the The Surgicalist Group’s vision.
4. Improved Surgical Outcomes
By eliminating significant wait time for surgery, surgicalists are able to prevent additional complications from occurring. In the case of someone needing a cholecystectomy (gallbladder removal) being sent home with medication to pacify the issue before seeing a surgeon, there is a chance their condition could worsen. Complications could include severe pain, jaundice, infection, and pancreatitis to name a few. The longer a patient waits for surgery to correct their condition, the higher the complications of their surgery ultimately leading to complications during surgery and a longer recovery time.
When a surgicalist is readily available, every day, ritually performing emergent and urgent general surgery cases, such as the cholecystectomy, patients no longer have to wait. Complications significantly decrease. Recovery time decreases. Length of stay decreases. Additionally, surgicalists are performing these types of general surgery cases routinely. The more surgical cases they do, the more efficient they become, and the more efficient the surgical teams become as they continue to work together. When surgical teams practice in a highly efficient manner, they know how to prepare the OR for the surgical tools the surgicalist will need, they can anticipate the surgicalist’s needs and work together in a seamless flow. As the OR teams ramp up their operational flow, the surgicalist refines his technique operating with better precision, ultimately leading to improved surgical outcomes.
Less time in the OR and precise technique often result in less surgical complications, fewer surgical site infections, and a lower number of readmissions of surgical patients.
5. Improved Bottom Line/Revenue Generation
We all know “time is money.” In a hospital setting, there certainly is no exception to this phrase. With a surgicalist model in place, hospitals experience efficiencies across the board.
Less time in the ED. Emergent and urgent surgical patients spend less time waiting in the ED. When they move to the OR, they free up a bed in the ED, allowing more emergency patients to be seen. ED volumes increase.
Less time in the OR. We’ve already touched on how the OR becomes more efficient with surgicalists in place. In doing so, surgical volumes increase as turn times decrease and unused block times are filled with emergent cases, making use of supplies and teams already available.
Increase in case capture and case mix index (CMI). With less distraction, Surgicalists have the time to to ensure proper documentation in and out of the OR. The likelihood that codes are missed, a commonality with rushed on-call surgeons, is rare. With proper case documentation improvement (CDI), hospitals see an increase in case mix index (CMI), directly impacting reimbursement rates, enhancing revenue generating opportunities for the hospital.
Shorter lengths of stay. Patients don’t wait with the surgicalist model in place. They get to the OR faster. Also, having a presence at the hospital 24/7 enables the surgicalists to round on their patients the next morning and expedite the discharge process.
Reduction in readmissions. Eliminating an extensive waiting period before surgery and reducing additional complications, paired with the surgicalist’s efficiency and precision in the operating room, all factor into a patient’s recovery, including minimizing any unnecessary returns to the hospital from complications due to surgery.
Elimination of call pay. Stop paying for surgical services that depend on a surgeon having to choose between his own elective practice and your emergent patient. Community surgeons are focusing on their elective cases. Surgicalists are focusing on your urgent and emergent cases.
Increase in elective surgical cases. With your community surgeons focusing on their elective practice, they no longer have the distraction of tending to emergent and urgent cases while they are on call. Additionally, if the surgicalist consults with a patient that does not need emergent or urgent surgery, they refer that patient to the community surgeon. These surgeons can plan their time better, see more elective patients – those who have already been waiting throughout the safer at home campaign and the new referrals – and conduct more surgeries.
Surgical volumes, as a whole, increase. Combining the increased elective cases from the community surgeons with the quick-turn emergent and urgent cases from the surgicalists, you can expect hospital surgical volumes to increase, as well.
Putting all these factors together reduces cost significantly.
We’re here to help.
As the veil lifts and elective cases resume, it is imperative that your patients get the care they need and deserve. We can help you, help your community surgeons, and your patients get back up to speed, performing better than ever. Connect with us.