Improved Outcomes, Decreased Length of Stay, and Increased Hospital Profits – The Surgicalist Model
Abstract
We evaluated the effect of implementation of a Surgicalist staffing model at a community hospital.
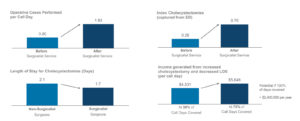
Under the Surgicalist staffing model we were able to increase the urgent case volume from 0.8 to 1.83/day. Index cholecystectomy capture rose from 0.26 to 0.8/day and their LOS decreased from 2.1 to 1.7 days. Complications requiring a readmission were decreased by over 30%. ED physicians satisfaction was drastically improved with the Surgicalist model regarding their interactions with the surgeon on-call as well as their confidence patients were getting proper care.
> $2.4M additional hospital income was captured off cholecystectomies alone because of the Surgicalist model.
Objective
To evaluate the effect of a dedicated Surgicalist service at a community hospital.
Summary
Acute Care Surgery (ACS) services are commonplace at academic hospitals with proven benefits. The volume of trauma, emergency general surgery and critical care patients is sufficient to warrant a dedicated surgical service to care for them. Some small and medium size hospitals across the country are experiencing challenges with surgical call coverage, issues with adhering to the latest trauma guidelines, and problems providing expedited, high quality care. Many centers have tried to remedy the situation by paying call stipends to surgeons in exchange for guaranteed coverage, however, this has done little to improve the problem and has led to other headaches.(1,2) Hospitals have discovered that simply scheduling coverage does not necessarily guarantee quality care and can become an additional expense without adding additional value.
With the increasing pressure of “pay for performance”, it is essential that we can quantify improved outcomes. A Surgicalist model solves these issues and generates increased income for the hospital in the process.(3)
Increasingly hospitals of all sizes and geographic locations are looking to reap the benefit of the ACS model but with a bigger emphasis toward the emergency general surgery portion of the model. This staffing model has demonstrated improved metrics regarding morbidity, mortality, length of stay, and 30- day readmissions.(4,5)
Methods
Prior to September 2017, a 220-bed community hospital utilized a traditional staffing model for Trauma and Emergency General Surgery call coverage. A Surgicalist service was then phased in to cover call days. From September 2017 through June 2018, a Surgicalist service was formed and utilized for approximately 30% of the call days. Starting July 2018, the service was expanded to cover approximately 75% of the general surgery call and 100% of all trauma call. Retrospectively we compared the data from all three periods of time. Length of stay (LOS), index case capture (cases taken to the OR directly from the ED), number of procedures performed, income generated for the hospital, complication rates, 30 day readmission rate, specific outcomes for cholecystectomies, and ED physician satisfaction. Data was acquired from the hospital’s EMR, by administration, and from a questionnaire emailed to the ED physicians via SurveyMonkey©.
Results
During the 13 months prior to the implementation of the Surgicalist service, 5 surgeons took a total of 382 days of call. An average of 0.8 cases were performed per call day, an average of 0.26 index cholecystectomies with an average LOS of 2.1 days. When the Surgicalist service covered 30% of the call days per month, that service performed of 1.42 cases per call day, 0.42 cholecystectomies with an average LOS of 1.7 days. When the Surgicalist service covered 75% of the call days, the number of cases per call increased to 1.83 with 0.7 index cholecystectomies. The national average DRG for an inpatient, uncomplicated cholecystectomy (DRG 419) is $8,0686. The average cost per day for a surgical bed, at for-profit hospitals in the area was $2,856.
With 30% call-day coverage by the Surgicalist service, the increase rate of index cholecystectomies added an additional $3,389 and the decreased LOS generated an additional $1,142 per call day. At 75% of the call days being covered, the Surgicalist service index cholecystectomy rate added $5,648 per day of call plus $1,142 in LOS savings. Essentially, for everyday the Surgicalist service took call, cholecystectomies alone generated an additional $6,790 for the hospital. This increased case capture adds a potential addition of $206,529 per month, over $2.4M per year, if 100% of the call days were covered by the Surgicalist service. The more call the Surgicalist group took, the more profitable it was for the hospital. These numbers are only looking at a single operation, obviously, this trend applies to other cases and the overall total income potential is much higher. (Table 1)
Complications that required hospital readmission within 30 days of discharge were evaluated during the first 8 months of 2018 (the data was limited to this time frame due to a change of electronic medical records in February of 2018). The Surgicalist group averaged 0.6 readmissions per month vs. the non-Surgicalist surgeons that averaged 0.9 per month. 30 day readmissions as well as wound complications and other adverse outcomes are closely scrutinized and will become even more so as the tiered provider system and pay-for-performance boundaries are tested.
Being amicable is an important trait in today’s surgeon. A large amount of hospital business comes through the emergency department and surgeons need to be ready and willing to help the emergency medicine physician triage and admit patients. A blinded survey was given to the entire emergency medicine physician group. They were asked to rate their satisfaction both BEFORE and AFTER the implementation of the Surgicalist model. A total of 12 of the 19 ED physicians responded with following results:
Q1 – BEFORE the implementation of the Acute Care Surgical Service, how satisfied were you with the approachability/responsiveness of the surgeons on call?
- 50% Satisfied
- 42% Dissatisfied
- 8% Neither Satisfied or Dissatisfied
Q1 – AFTER the implementation of the Acute Care Surgical Service, how satisfied were you with the approachability/responsiveness of the surgeons on call?
- 83% Very Satisfied
- 17% Satisfied
- 0% Dissatisfied or Very Dissatisfied
Q2 – BEFORE the implementation of the Acute Care Surgical Service, how satisfied were you with the ease/speed of admitting patients to the surgeons on call?
- 58% Satisfied
- Dissatisfied
- Neither Satisfied or Dissatisfied
Q2 – AFTER the implementation of the Acute Care Surgical Service, how satisfied were you with the ease/speed of admitting patients to the surgeons on call?
- 83% Very Satisfied
- 17% Satisfied
- 0% Dissatisfied or Very Dissatisfied
Q3 – BEFORE the implementation of the Acute Care Surgical Service, how satisfied were you with the surgical care/expertise of the surgeons on call?
- 67% Satisfied
- 17% Dissatisfied
- 16% Neither Satisfied or Dissatisfied
Q3 – AFTER the implementation of the Acute Care Surgical Service, how satisfied were you with the surgical care/expertise of the surgeons on call?
- 58% Very Satisfied
- 42% Satisfied
- 0% Dissatisfied or Very Dissatisfied
Q4 – BEFORE the implementation of the Acute Care Surgical Service, what was your overall satisfaction with the surgical service?
- 42% Satisfied
- 42% Dissatisfied
- 16% Neither Satisfied or Dissatisfied
Q4 – AFTER the implementation of the Acute Care Surgical Service, what was your overall satisfaction with the surgical service?
- 67% Very Satisfied
- 33% Satisfied
- 0% Dissatisfied or Very Dissatisfied
Discussion
General surgery has gone through many changes in the last few decades. The broad based practice in which a surgeon could comfortably perform thoracic, vascular, urologic, oncologic, and gynecologic surgery is practically a thing of the past. Specialists, and sub-specialists have emerged and pulled large numbers of patients from the community general surgeon leaving them to balance what is left to maintain a lucrative practice. Taking “call” used to be a way to bring patients into your practice, secure elective cases, and create a revenue stream. Due to many factors, including insurance contracts, increased ED volumes, decreased reimbursement, high rates of underinsured patients, being on-call, is often much more work than it is worth for surgeons with elective practices. When on call, surgeons are often up most of the night dealing with situations that will yield them little to no income while fatiguing them for the next day – a day that might be filled with scheduled cases, endoscopies, or an office full of patients. Add to all of that the scrutiny of patient satisfaction surveys, the frustrations of electronic medical records, and the ever-increasing amount of paperwork. These issues have created a challenge for small and medium sized hospitals to achieve consistent surgical call coverage. Patients that could be appropriately admitted and taken to the OR the same day they are seen in the emergency department are often sent home and evaluated at a more convenient time for the surgeon, or transferred to other facilities. This lack of appropriate care leads to loss of revenue for the hospital, slower throughput for the ED, and most importantly it provides sub-standard patient care.(5)
The Hospitalist specialty was developed decades ago to address the similar challenges Internal Medicine was facing: balancing inpatient and outpatient practices, excessive patient length of stays, complication rates, and physician satisfaction. These issues are mirrored in today’s general surgery practice and unfortunately, these challenges affect the bottom line for the healthcare system. When outside factors decrease the speed and efficiency of the care of the patient, LOS is increased, complications are increased, satisfaction is decreased, and reimbursement is decreased. By solely focusing on inpatient care of the surgical patient, outcomes and profits are improved just as they did under the Hospitalist model.
Michael Porter, MBS, author of Redefining Health Care: Creating Value-Based Competition on Results, spoke at the American College of Surgeons this year (2018) regarding the need to restructure healthcare. His main solution revolves around looking for value-based solutions, ones that are proven to add to the bottom line either by decreasing complications or by increasing revenue. He is vocal proponent of spending money on quality in order to achieve improved outcomes.
Conclusions
The Surgicalist model is a benefit to hospitals. We were able to demonstrate lower complication rates, lower readmission rates, improved patient retention through higher index case capture, an increase in total number of cases performed, improved satisfaction of referral physicians and increased revenue for the hospital. While more evaluation is needed, this is now the second data review, from separate states, at different sized hospitals that show the Surgicalist model is providing better patient care while at the same time helping hospitals with their bottom line.
Download the complete document:
1. O’Mara M, Sherer L, Wisner D. Sustainability and Success of the Acute Care Surgery Model in the Non Trauma Setting, JACS.2014;219(1):739-44.
2. On-Call Crisis: A Statewide Assessment of the Cost of Providing On-Call Specialist Coverage, Ann Emergency Med.2007;49(6):227-233
3. The Surgicalist Method: Better Workflow, Better Care, Better Bottom Line. Becker’s Hospital Review, 2015
4. Oliver Wyman Healthcare Cost and Utilization Project, 2016, Performed for The Surgicalist Group
5. To K, Kamdar N, et al. Acute Care Surgery Model and Outcomes in Emergency General Surgery, JACS, 2018;07(664):21-8
6. Pushwaz W, Paranjape C. Variation in National DRG Payments for Laparoscopic Cholecystectomy: Hospital Level Analysis, SAGES, www.sages.com
7. Ellison, A. Average Cost per Inpatient Day Across 50 States. American College of Surgeons Communication 2018
Authors:
Casey Thomas, DO, FACS, FACOS, Chief Medical Officer, The Surgicalist Group
David Terry, DO, Chief Operating Officer, The Surgicalist Group
Bruce Curran, Vice President of Finance, The Surgicalist Group
Mit Desai, MD, FACS, Founder and CEO, The Surgicalist Group