Better Workflow. Better Care. Better Bottom Line.
Written by Mit Desai, MD FACS, Founder and CEO, The Surgicalist Group | Published online by Becker’s Hospital Review
The necessity of adopting new delivery models that improve patient care while increasing patient throughput, is felt from the top down.
Before adopting a new model, however, the importance of offering evidence of the model’s success is paramount. One such model which is gaining traction establishes a new way to execute ED surgical staffing, promising better departmental workflow, better patient care, and a better bottom line for hospitals in response to the growing demands placed on hospital administrators. Furthermore, over the last eight years of instituting the surgicalist model in hospitals across the nation, hospitals have collected enough data to show that this particular delivery method has grounds to last.
First, the essential question: What is a surgicalist? When considering this model, it is important to forget nearly everything about the traditional way of staffing an ED surgical department. Surgicalists are general surgeons by training and receive the same training as a traditional “community” surgeon, and possess identical capabilities to that of a traditional surgeon; however, there are fundamental differences, not only in where they practice, but how they practice in comparison. Surgicalists work only within a hospital and their practice centers on emergent care of patients, with no elective patients outside of the ER. Their 24/7 availability when they are on call allows for dedicated scheduling, ensuring at a surgicalist-staffed hospital, that there is always a surgicalist available to take ED surgery cases. As a result, community surgeons are freed to focus solely on their elective practice, maximizing their time in their respective offices and minimizing commute time to hospital ERs.
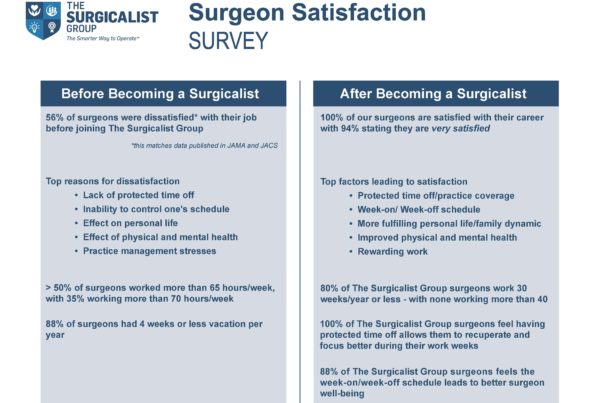
Surgicalists are on-call for a full seven days and then off for seven days. During their seven days on, they are not juggling an elective practice with their ED duties, enabling them to be well-rested and involved members of a hospital team. They are able to offer optimal care to their patients in the ER, and have opportunities to pursue professional development at the same time because of their significant time off. This development translates to a more involved surgical staff member in the big picture of the hospital.
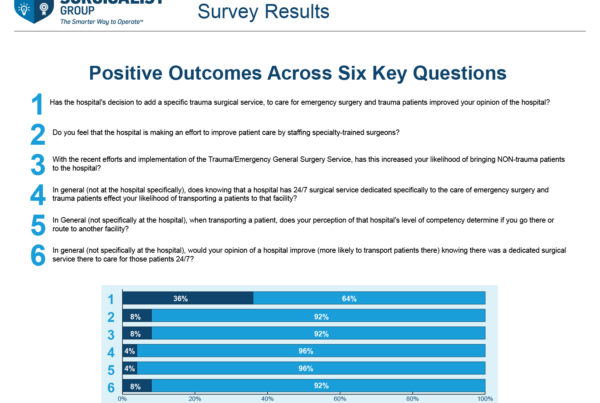
Not only are there interdepartmental benefits on a large scale, but dedicated surgical staffing makes the actual ED department more efficient at treating and discharging patients. All of our measured hospitals with this model indicate shorter length of stay by surgicalist patients compared to the rest of the surgical population in each hospital. EDs with surgicalists move toward better throughput, which only increases a department’s capacity to see more patients, and transfer fewer of those it sees.
In addition, patients get better faster when treated by surgicalists, and have improved outcomes compared to those treated by the general surgeon population in the same hospital. Patients treated by surgicalists have significantly fewer complications than those by hospital peers. They also have fewer 30-day readmissions and fewer seven-day readmissions, and lower risks of mortality. These are some of the most crucial metrics for which hospital leadership is held accountable.
Another major concern is hospital acquired conditions (HACs). Surgicalists have fewer overall cases of HACs, namely falls and trauma (HAC5), vascular catheter-associated infections (HAC7), and Iatrogenic pneumothorax with venous catheterization (HAC14).
When an emergency department performs better on HACs, this represents a safer environment for the entire patient population in that hospital. This all represents good patient care news for hospital leadership considering the model.
The final factor worthy of hospital administration awareness is the better bottom line. We have found that hospitals with surgicalist programs enjoy lower average total costs, lower average variable costs, lower average observation charges, and lower emergency department charges. It is evident that the surgicalist model not only reduces costs to hospitals in the emergency department, but the effects are felt on a larger scale as well, making the program a novel way to cut costs while improving workflow and patient care, all in concert. Considering the fact that many cost-cutting procedures have the opposite effect on departments and the patients in their care, this represents a unique opportunity to hospital leadership.
Hospital executives are forced to make difficult decisions every day. The intent of sharing these findings is to make one decision easier. The ED can often be a source of some of the longest wait times in hospital systems, staining the reputation of an otherwise efficient institution. Staffing troubles in the emergency surgical department can similarly be a serious headache to not only administrators, but the surgeons themselves.
More hospitals are increasingly adopting the surgicalist model, and preliminary findings indicate there may be very good reasons for more to follow suit. The surgicalist model represents the future of emergency surgical departments, and it is essential for hospitals to quickly begin leveraging the model for the benefits it yields to patients and bottom lines, alike.
Mit Desai, MD FACS, is the Founder and CEO of The Surgicalist Group. A graduate of The Wayne School of Medicine in Detroit, Dr. Desai completed his general surgery residency at The University of Illinois before moving to Florida and founding his own surgical practice. In 2006, Dr. Desai began exploring the emerging concept of the “surgicalist” form of practice. Finding an opportunity to partner with hospitals, Dr. Desai founded The Surgicalist Group, delivering an innovative, in-hospital acute care surgery model to hospitals nationwide.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
© Copyright ASC COMMUNICATIONS 2020. Interested in LINKING to or REPRINTING this content? View our policies by clicking here.
Read you may also read The Surgicalist Method: Better workflow, better care, better bottom line directly on Becker’s Healthcare Review site.