For your hospital, having a general surgeon on call 24 hours a day, seven days a week for the emergency department (ED) is a necessity. Relying heavily on your community general surgeons or employed general surgeons to address the emergent and urgent surgical needs of patients when they come to the emergency department is a pivotal access point in the care process. Relying on community surgeons for ER-call negatively impacts throughput of your hospital in all directions. There is a smarter way to approach the emergency call model that requires understanding the psychology of on-call surgeons, something I know firsthand.
Over 13 years ago, as a general surgeon with a busy private practice, I was seeking a better approach to delivering surgical care. Like most, I was passionate about being a surgeon, but was juggling a loaded clinic schedule and a busy elective surgery schedule. On top of it all, I took ER-call to build my practice, as I was starting out. I worked hard; 24/7 and nearly 365 days a year in the first few years as I built my practice. Disillusioned with little personal time for me or my growing family, I realized something had to change. And, talking with my general surgery peers, I was not alone in my frustration and impending burnout. I was doing my best, but the burden was taking a toll. There was always someone I was disappointing. My patients on the clinic schedule for consultations, pre-op, or post-op visits often had to wait for me if my scheduled surgeries ran late or I was called to the OR for an emergent or urgent case. The patients who came to the ED needing emergent surgery had to wait for me and were often boarded in the halls of the ED until I could make it back to the hospital after a long day of seeing patients in my clinic. My family was disappointed when I could not make it home for dinners or events. I was frustrated with having little to no time for myself to live a healthy, balanced life.
Time for a New Approach for ER-Call
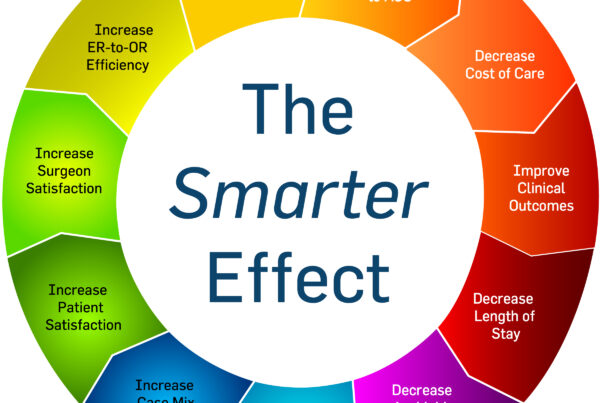
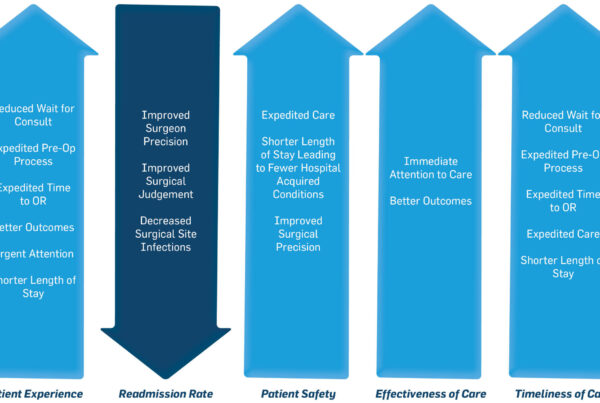
Realizing that a lifetime of managing both a private practice and a hectic ER-call schedule was less than desirable, I took a deep look at what drove me at my core. I wanted nothing more than to be in the OR taking care of patients along with a more harmonious balance between my work and personal life. My strategy was to shift away from elective cases and focus on ER-call for my community surgeon colleagues. This approach was like the hospitalist model for inpatient care that started in the late 1990’s. I wanted to create a similar model to the hospitalist, consulting on the patient in the ED, schedule them for surgery, and manage their hospitalization course. Like the hospitalist model, I wanted to implement a block schedule to address the issues of burnout and patient satisfaction. As I started to adopt this approach for emergent and urgent surgery with another general surgeon in our community, we saw our practice grow organically to local hospitals in the Tampa, Florida market. Something else happened that was a byproduct of our new approach. The hospitals reported seeing positive changes in patient experience scores, OR utilization, throughput, reduced cost of care and length of stay, and excellent clinical quality outcomes metrics for our cases. The CMI for hospitals began to increase and case capture shot higher. Our dedicated on-call services included incorporating consistency in our approach, working with the hospitals on improving throughput, processes around discharge planning, and other small but important process improvement. Our services were in high demand and we started to expand in Florida. The momentum in the demand for our model led to referrals to start programs in other states, which led to the formation of The Surgicalist Group.
Ironically, around the same time, on the other side of the globe and in a different industry, Sir Dave Brailsford, the head of the British Cycling team was implementing the strategy of ‘aggregated marginal gains,’ to improve the team’s performance. Historically, the team had earned just one Olympic gold medal over its 76 years of competition. Brailsford, taking an unorthodox approach, took to dissecting every element of the team with the goal of applying just a 1% improvement to each part. The thought was that by making numerous small improvements, the aggregate result would advance the team to the “gold.” He was right. In 2008, at the Beijing Olympics, the British Cycling team won 10 gold medals.
At its highest level, Sir Brailsford’s’ recipe for success seems simplistic and direct: small improvements across the board, resulting in overall improved outcomes. But determining where to start, and how to allocate the manpower to several small tasks requires direction, coordination, and collaboration to truly succeed. If the core were ignored, the entire project could implode. If everyone were not aligned and held accountable for the results, the disconnect would lead to failure. Brailsford attributed teamwork as the glue that lead to the team’s success.
There is something to be said about having the right team in place, especially with respect to the ER-call model. The Surgicalist Group’s smarter way to approach the emergency call model takes this into account. Keeping your ED and OR teams aligned and accountable for operational and surgical outcome goals requires dedication and coordination. With elective surgeries returning in the post-COVID-19 surgical surge, general surgeons are more focused on their elective practice than ever before, working down their backlog from the past three months and rebuilding their referrals. Shifting ER-call to surgicalists to cover emergent and urgent surgery 24/7 frees up the general surgeon and ultimately benefits their patients, the hospital, and the surgeon’s well-being.
If you’d like to see what financial benefit The Surgicalist Group’s model offers your hospital, go to the calculator on our website (scroll down to the bottom of our homepage) and you can estimate the potential financial gain. Then, we can schedule a time to explore specific areas of performance where we can help optimize your hospital’s ED and surgical services.
by Mit Desai, MD, FACS, Founder and CEO of The Surgicalist Group